Partnerships
Project on Breastfeeding and Newborn Care

How is a unique partnership creating a Bahraich Model of care for LBW babies?
The Project’s work with low birthweight and premature babies is closely aligned with the National Health Mission’s Kangaroo Mother Care and Optimal Feeding of Low Birthweight Infants Operational Guidelines. The Family Participatory Care and Facility Based Newborn Care Guidelines also guide the Project. The Project improves on the care described in the Home Based Newborn Care Guidelines by providing community follow-up by trained nurses rather than ASHAs.
Achievements
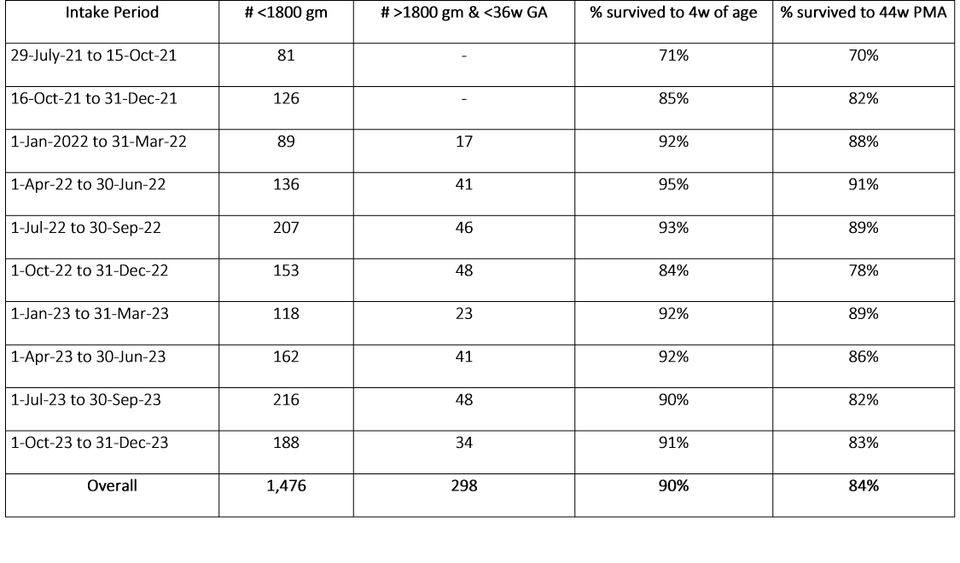
Between August 2021 and December 2023, the Project on Breastfeeding and Newborn Care served about 1,770 babies who were less than 1800 grams or less than 36 weeks GA. This is approximately 61 new babies per month. They benefited from the ASMC Bahraich’s SNCU, its 17-bedded KMC wards, and from phone calls and home visits from trained nurses. One-month mortality for these babies, who include LAMA, abscond, and referred out cases was about 1 in 10.
Informed by the Government of India’s KMC, FBNC, and FPNC Guidelines, the Bahraich Model of care is a unique partnership between the ASMC Bahraich, a medical college in eastern Uttar Pradesh, and r.i.c.e., a not-for-profit focused on child health.
The program has facilitated:
- An increase in the number of Kangaroo Mother Care (KMC) beds for stable low birth weight (less than 1800 gm) and premature (less than 36 weeks) babies.
- An increase in nursing staff to establish mother’s milk supply, and to train parents to feed a LBW baby, give KMC, prevent hypothermia, and recognize danger signs.
- An increase in the frequency of community follow-up using phone calls and home visits to monitor weight gain, temperature, and identify problems.
- When a child shows danger signs during community follow-up, the nurses suggest to the family to call the public ambulance and take the infant to the nearest public hospital.
Activities
The Project comprises four key components:
- Hospital Arm: Screening and counseling
Each day, a nurse counselor screens babies in ASMC Bahraich. She identifies mothers for breastfeeding support and provides counseling. She also identifies babies under 1800 grams or less than 36 weeks of gestation, and takes them to a pediatrician at the Special Newborn Care Unit (SNCU). If the SNCU pediatrician and the mother’s doctor recommend it, the baby and mother are shifted to a KMC ward. Nurse counselors explain the program to families and take their consent for program participation and to record their information.
A nurse screens babies in the post-natal care ward.
- Hospital Arm: Bed-side care for premature and LBW newborns
The program provides trained nurse counselors, who work under the supervision of SNCU pediatricians, to the two KMC wards around the clock. Ward Assistants support mothers who are expressing milk or learning to tie KMC wraps. In order to facilitate KMC, the staff give a gown, a thermometer, a KMC wrap, and a baby cap for each baby in the program. If the baby can feed at the breast, no further supplies are needed. However, if the baby needs to be fed expressed milk, the staff will also give kathori, spoon, tiffin, and/or a nifty cup.
The nurse counselors maintain records about the babies’ weights, temperatures, KMC hours, and feeding. She also teaches caregivers how to safely feed expressed breastmilk when needed. If a baby is unable to take oral feeds and the pediatrician orders an infant feeding tube (IFT), the nurse counsellor takes the family’s consent for IFT feeding. Then, she inserts the IFT and administers feeds as per the doctor’s orders. She monitors babies for signs of distress and sends babies who need it to the SNCU for consult and/or stay. She works under the supervision of the SNCU pediatricians.

Nurse teaching how to safely feed expressed breastmilk.

A nurse teaches a mother to tie the KMC Wrap.
- Phone / Home Arm: Follow-up phone calls
After families exit the hospital, a nurse counselor contacts them to see how the mother and baby are doing. The frequency of contact with the family depends on the condition of the baby. For example, most babies under two weeks old, and those who experience slow growth, or are at risk of slow growth, are called daily. Healthy, breastfed infants who are over 1800 grams and over two weeks old are contacted one per week.
During follow up calls, the nurse counselors give breastfeeding encouragement and advice, and remind families to look for danger signs. Families receive weighing scales and thermometers as part of their program participation. Nurse counselors ask the families to report the babies' temperature and weight on the phone call.
Phone calls help the staff assess whether a baby is experiencing hypothermia, suboptimal weight gain, or weight loss. Based on the baby’s hospital record and information gleaned during phone calls, the phone and home managers decide which babies would benefit from a home visit. Families who cannot be contacted for a certain period receive a visit from a nurse counselor.

A nurse observes a baby on a home visit.
- Phone / Home Arm: Home Visits
Nurse counselors make home visits to babies whose families need additional counseling to establish breastfeeding or encouragement to seek care. On each home visit, after taking the family’s consent, the nurse assesses the baby, and provides advice tailored to the baby’s vital signs, weight trajectory, and feeding abilities. Home visits are also done for babies who otherwise are not showing any signs of distress, and yet show inadequate weight gain. For such babies, nurse counselors do home visits to assess milk supply, feed frequency, duration and quantity, and then provide feeding advice to the mother. They also encourage families to maintain hygiene and give the newborn lots of KMC at home.
Outcomes
Between August 2021 and December 2023, the Project on Breastfeeding and Newborn Care served about 1,770 babies less than 1800 grams or less than 36 weeks GA. This is approximately 61 new babies per month. Between August 2021 and April 2022, the program primarily included babies born with a birthweight less than 1800 grams. However, we realized that those born more than 1800 grams but less than 36 weeks gestation are also at high risk of feeding difficulties. Therefore, in May 2022, we changed the program criteria to include babies less than 1800 grams or less than 36 weeks gestation.
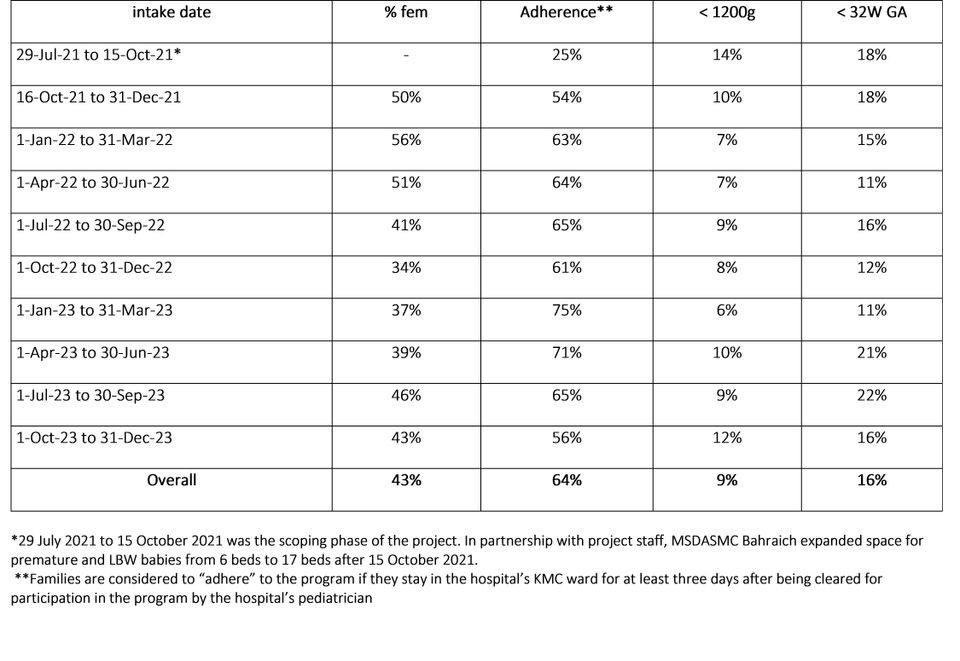
The first table summarizes the number of participating babies and their mortality rates by period of intake. The second table summarizes characteristics of babies recruited in each time period. Table 1 shows seasonal variation in participation and survival. Table 2 shows that boys are overrepresented in the program relative to girls.
Number of babies participating in the Project, by quarter
Characteristics of babies less than 1800 grams or less than 36 weeks GA who participated in the program, by quarter
Learnings
While developing the Bahraich Model of newborn care in partnership with ASMC Bahraich, Project staff have learned valuable lessons about reducing mortality among premature and LBW babies.
It’s time to incorporate gestational age into newborn care guidelines
The NHM’s KMC Guidelines were published in 2014, when fewer mothers had been to school, and fewer mothers were getting antenatal care. The KMC guidelines rely on weight, an observable indicator, to guide a baby’s care. However, as a result of changes in women’s education and the availability of ANC, most mothers, even in poor rural settings, know their LMP or have had an early ultrasound. This allows pregnancy dating. Because a newborn’s development and needs are related to both her weight and her gestational age, we suggest that government guidelines incorporate both weight and gestational age.
Following feeding guidelines for LBW and premature infants takes a lot of hands
The most recent Facility Based Newborn Care Guidelines say that all LBW and preterm babies who are stable should be receiving breastmilk from the first day of life. However, most cannot feed at the breast in the first few days of life. Milk must be expressed, stored, prepared, and fed to them, either using a cup and spoon, or an infant feeding tube. They need to be fed this way every two hours for the first several weeks of life. It takes many trained nurses, as well as support staff, to guide mothers through this period, and to ensure babies are fed safely and are growing well.
Trained nurses can improve home-based care
The Home-Based Newborn Care Guidelines make provisions for ASHAs to visit the families of LBW and premature babies after they exit the hospital. Because LBW and premature babies have special needs that are different from the needs of normal weight and full-term babies, trained nurse counselors are better able to provide follow up care and referrals for this group of babies. The Project has developed unique templates for home visits that follow a baby from hospital exit to 44 weeks postmenstrual age.
Improving newborn outcomes requires increasing families’ demand for care
Despite the fact that most parents want what is best for their children, lack of demand for evidence-based care for LBW babies is a key constraint for health providers in rural Uttar Pradesh. Some parents do not understand that LBW reduces the chances of survival, others do not understand that KMC and breastmilk feeding can be as important as medicines. Others hold superstitious beliefs and are suspicious of modern medicine. It is important for health providers to connect with each family, and explain, in terms specific to their child, the benefits of seeking specialized premature and LBW newborn care.
Success: What is it like?
Rupa and Amit’s baby girl was born at 28 weeks gestational age. Her parents learned to feed her expressed breastmilk, and did 14 hours of KMC per day. The parents were trained to recognize warning signs. The team visited Rupa and her baby at home and helped the baby learn to feed at the breast when she reached 34 weeks postmenstrual age.

Rupa and Amit’s baby girl.
Rani Singh and Ram Kumar’s baby was born at 33 weeks. His mother was very worried because she had already lost four children to premature birth. The baby received medications and phototherapy from the SNCU, and counseling on feeding expressed breastmilk and doing KMC from the Project staff. When he attended the facility-follow up at ASMC at 4.5 months corrected age, Rani and Ram’s baby was the picture of health.

Rani Singh and Ram Kumar’s baby.